Why Your Gut Health Might Be Controlling Your Weight
Gut health isn’t just a buzzword anymore—it’s become a cornerstone of wellness for anyone serious about weight management. Across the globe, both nutrition experts and wellness enthusiasts are turning their focus inward, literally, to a complex community of bacteria, fungi, and other microorganisms living in the digestive tract. This vital internal ecosystem, known as the gut microbiome, is proving to be a game-changer in understanding how our bodies process food, store fat, and regulate appetite.
In this blog, I’ll guide you through how your gut—home to nearly 100 trillion microbes—might be quietly controlling your weight more than your calorie tracker ever has. From appetite signals to fat storage patterns, we’ll explore the intricate ways your microbiome might be influencing your waistline without you even realising it. And more importantly, we’ll discuss how you can optimise your gut health using simple, science-backed strategies that are central to Claudia’s Concept.
The Gut Microbiome: Your Body’s Hidden Weight Regulator
Trillions of Microbial Allies Living Inside You
When we think about weight management, we often focus on calories, macronutrients, or maybe our workout routine. But hidden deep in our digestive tract lies a powerful system that silently shapes the way we gain, lose, and maintain weight—the gut microbiome. This dynamic ecosystem, composed of more than 100 trillion microorganisms including bacteria, viruses, and fungi, communicates directly with our metabolism, immune function, and even brain signals related to hunger and satiety.
The diversity and composition of your gut flora influence how your body processes food, stores fat, and uses energy. In fact, emerging research from institutions like the National Institutes of Health and Harvard T.H. Chan School of Public Health has highlighted the microbiome as one of the most pivotal regulators of energy balance and body fat composition.
Gut Bacteria and Your Body’s Energy Budget
Let’s break this down. Different bacterial strains in your gut hold different metabolic capabilities. Some strains, particularly from the Firmicutes phylum, extract more calories from the food you eat, while others, like many found in the Bacteroidetes phylum, are less efficient in this high-energy harvest. A study published in the journal Nature found that obese individuals typically have a higher Firmicutes-to-Bacteroidetes ratio compared to lean individuals, meaning more calories are absorbed—a direct influence on body weight.
So if you’re eating the same amount of food as someone else, but your gut has more energy-extracting bacteria, your body will naturally absorb more calories. This isn’t about willpower—this is biology driven by your gut’s microbial fingerprint.
Your Internal Weight-Stabilizing Mechanism
A balanced and diverse microbiome doesn’t just passively exist—it actively mediates hormone production, inflammation levels, fat storage signals, and blood sugar regulation. A well-regulated microbiome improves insulin sensitivity, reduces low-grade inflammation, and supports lean body mass maintenance. Studies in Cell Metabolism show that increasing microbial diversity, especially through diet and lifestyle changes promoted by Claudia’s Concept, leads to a measurable reduction in body fat percentage—without major shifts in calorie intake.
Let’s not forget the microbiome’s role in regulating appetite through signals to the brain. Certain bacteria produce short-chain fatty acids (SCFAs) like butyrate, which increase the body’s production of satiety hormones like GLP-1 and PYY. This process helps you feel full and satisfied, reducing overeating tendencies.
Why a Balanced Gut Keeps Weight Gain in Check
Think of your gut microbiome as your body’s internal thermostat for weight. When it operates in harmony, it prevents excessive fat build-up, optimizes energy usage, and aligns hunger cues with true nutritional needs. But when imbalances occur—often from poor diets, stress, antibiotics, or lack of sleep—the wrong microbes take over and shift your metabolism toward fat storage rather than fat burning.
At Claudia’s Concept, we focus on personalized gut-healing strategies that recalibrate this microbial balance, aligning your body’s natural systems to support healthy weight. Through gut-focused nutrition, we help reintroduce the right species, encourage microbial diversity, and restore the hidden ecosystem that could be the missing link in your wellness puzzle.
So now ask yourself—what if your journey to long-term weight stability isn’t only about eating less, but nourishing your gut more?
Probiotics and Prebiotics: Feeding the Right Bugs
What Are Probiotics?
Probiotics are live, beneficial bacteria that play a direct role in your digestive and metabolic health. You’ll find them naturally in fermented foods like yogurt with live cultures, kefir, miso, sauerkraut, kimchi, and kombucha. When consumed consistently, these friendly microbes colonize your gut, helping to maintain a healthy balance of gut flora. It’s not just about digestion—they actively influence your weight by modulating how your body stores fat, responds to hunger, and processes calories.
Research published in the journal Obesity Reviews shows that certain strains of probiotics, such as Lactobacillus gasseri and Bifidobacterium lactis, can reduce body weight and body fat percentage. In clinical trials, people taking Lactobacillus gasseri saw abdominal fat reduced by up to 8.5% over 12 weeks without changes to diet or exercise. That’s the power of feeding the right bugs.
What Are Prebiotics?
While probiotics are the living microbes, prebiotics are the fuel that keeps them thriving. These are non-digestible fibers found in whole foods like chicory root, garlic, onions, leeks, asparagus, and green bananas. You can’t digest them, but your good gut bacteria can—and they love them.
Think of prebiotics as the fertilizer for your internal garden. Without them, even the healthiest probiotics won’t flourish. At Claudia’s Concept, I always encourage including both in your daily nutrition to ensure the gut ecosystem stays balanced and active. A diverse microbiome depends on consistent nourishment through these powerful prebiotic fibers.
How They Impact Digestion and Weight
The synergy between probiotics and prebiotics is where the real magic happens. This dynamic duo improves gut motility, supports efficient nutrient absorption, and even boosts short-chain fatty acid production—which has been linked to reduced fat accumulation and improved insulin sensitivity.
A 2020 study in The British Journal of Nutrition found that prebiotic supplementation (specifically inulin-type fructans) significantly improved satiety hormones like GLP-1 and PYY, which help regulate appetite and energy intake. This hormone shift leads to fewer cravings, better portion control, and ultimately, healthier weight management.
Furthermore, these gut-loving nutrients promote microbial diversity. An increased variety of species leads to an anti-inflammatory environment—a crucial factor since inflammation is deeply tied to fat storage and metabolic dysfunction. At Claudia’s Concept, we take a targeted approach: balancing the microbiome isn’t just about variety, but also about having the right species active and supported by the right foods.
Have you ever noticed changes in digestion, mood, or weight after a few weeks of eating more plant-based, fermented, or fiber-rich foods? That’s your gut microbiome responding. It adapts, evolves, and either supports or sabotages your goals based on how you feed it. So the next time you reach for something to eat, ask yourself: are you feeding your hunger, or your microbes?
Gut Flora and Digestion: Breaking Down More Than Food
What if I told you that your gut flora doesn’t just digest your food—it actually helps determine how many calories you absorb and how efficiently your body uses them? That’s the reality revealed by current science. At Claudia’s Concept, this principle forms a critical foundation for weight management strategies that go beyond calories and into cellular-level efficiency.
Gut Bacteria: The Microscopic Digestive Workforce
Your gut hosts trillions of microbes—predominantly bacteria—that carry out metabolic duties no human cell can perform. These microbes break down complex carbohydrates, ferment dietary fibers, and synthesize short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. These SCFAs don’t just fuel your colon cells; they impact your metabolism system-wide.
For example, research published in Nature Reviews Gastroenterology & Hepatology shows that SCFAs regulate fat storage by activating AMP-activated protein kinase (AMPK), which increases fat oxidation and reduces fat storage. That means the better your digestion via healthy gut flora, the more your body becomes a fat burner rather than a fat hoarder.
When Flora Goes Foul: Poor Gut Health’s Effect on Digestion and Metabolism
Unbalanced gut flora—often called dysbiosis—can wreak havoc on digestion. It reduces the body’s ability to properly break down and absorb nutrients, causing bloating, gas, constipation, and chronic discomfort. But digestion problems aren’t just inconvenient—they slow down your metabolic engine.
Here’s how: An unhealthy gut increases gut permeability, which triggers a cascade of immune responses and systemic inflammation. This can impair hormonal signals like insulin and leptin, two of the most critical regulators of fat storage and hunger. The result? A sluggish metabolism and an uphill battle with weight gain.
Digestive Efficiency = Caloric Burn Efficiency
You might be surprised to learn that how efficiently you digest food directly impacts how many calories you burn. Studies published in Cell Metabolism found that individuals with a diverse, balanced gut microbiome had more stable energy expenditure and better blood glucose control. That translates to fewer blood sugar crashes, reduced cravings, and a body primed to burn fuel smoothly rather than store it.
At Claudia’s Concept, I integrate gut flora optimization into 360° wellness programs. If your digestion feels heavy or energy levels keep crashing, your microbiome could be signalling imbalances. The good news? You can shift your internal ecosystem towards harmony with tailored nutrition, prebiotic-rich meals, and conscious food combining strategies.
Think about it—when your digestion flourishes, your whole system operates in harmony. So, how in tune is your gut with your goals?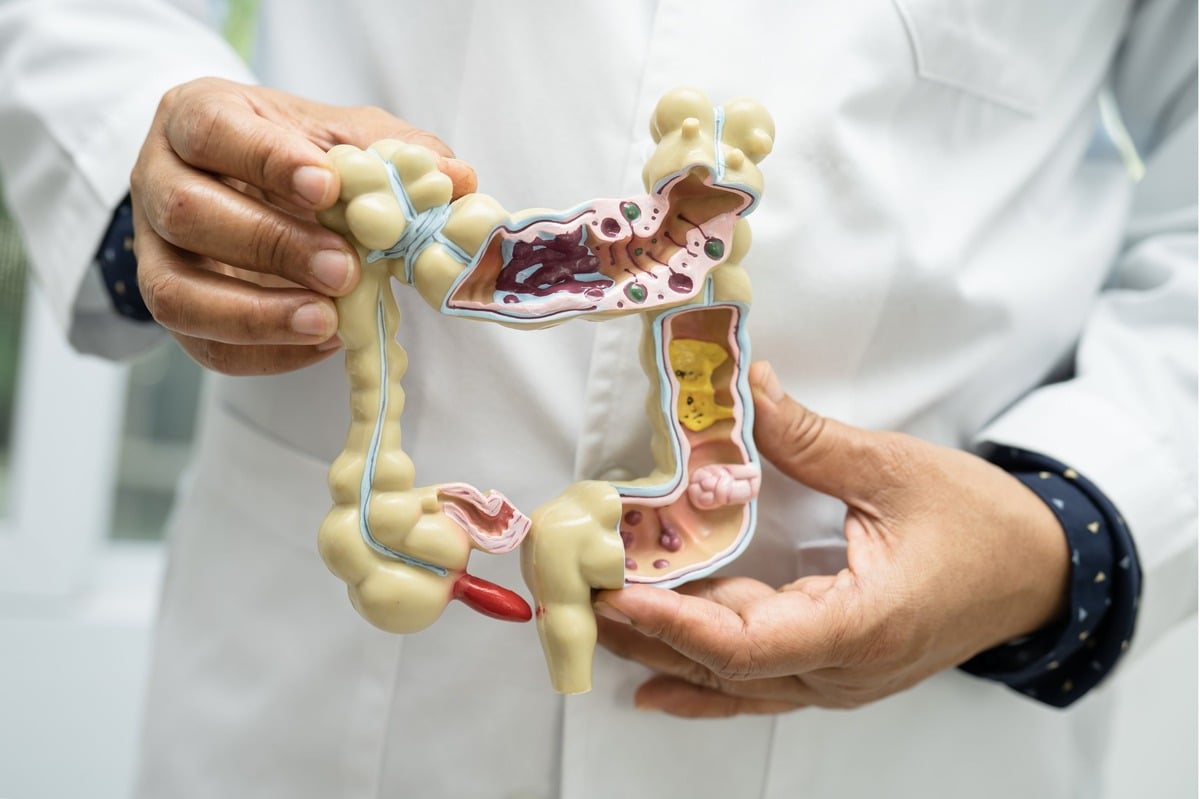
Inflammation and Gut Health: The Role of Chronic Inflammation in Weight Gain
You’ve probably heard the term “inflammation” being tossed around in conversations about health and diet. But what does it really mean for your weight and your gut? If you’re struggling with stubborn fat—especially around your belly—it’s time to take a hard look at what’s happening beneath the surface. In the world of nutrition science, chronic inflammation is no longer seen merely as a silent symptom. It plays an active, decisive role in how your body stores fat, manages blood sugar, and even perceives hunger.
So, What Exactly Is Chronic Inflammation?
Chronic inflammation is a prolonged, low-grade immune response that continues to signal your body’s defenses even when there’s no real threat. Unlike acute inflammation—think swelling when you bump your knee—this type subtly simmers for months or even years. The gut is one of the most common sources of this condition, especially when the microbial balance is disrupted.
When harmful bacteria gain dominance due to poor diet or stress, the gut lining becomes irritated. This irritation stimulates immune activity, triggering an inflammatory cascade. Your body goes into a continuous state of mild alarm, draining energy and resources. This doesn’t just affect your immune system—it transforms your metabolism, too.
Inflammation’s Direct Link to Metabolism and Fat Storage
Let’s decode how chronic inflammation literally rewires weight regulation. Elevated inflammatory markers—especially cytokines like TNF-α and interleukin-6—alter insulin signaling. These changes reduce insulin sensitivity, a condition known as insulin resistance. And here’s the kicker: insulin resistance leads to higher blood sugar and increased fat storage, particularly visceral fat around the abdomen.
According to a 2020 review in the journal Cell Metabolism, this process also diminishes your body’s ability to burn fat for fuel. Essentially, your body becomes locked in fat-storing mode. Combine that with lowered leptin sensitivity (leptin is your fullness hormone), and it’s easy to see how chronic inflammation promotes both overeating and higher fat retention.
Pro-Inflammatory vs. Anti-Inflammatory Foods: What You Eat Shapes Your Gut
Food is not just fuel—it’s information. With every bite, you’re sending signals that either aggravate or soothe your gut environment. Diets high in saturated fats, refined sugars, and ultra-processed foods increase the concentration of Gram-negative bacteria in the gut. These bacteria release lipopolysaccharides (LPS), inflammatory toxins that enter the bloodstream when your gut barrier is weakened.
On the flip side, anti-inflammatory foods operate like natural healers. Omega-3 fatty acids (found in flaxseeds, walnuts, and fatty fish), polyphenols (abundant in berries, green tea, and olive oil), and dietary fiber from vegetables actively reduce gut inflammation. A 2019 study in Frontiers in Immunology showed that subjects consuming a Mediterranean-style diet—rich in these anti-inflammatory heroes—had significantly lower markers of systemic inflammation and healthier waistlines to show for it.
Claudia’s Concept: Tackling Inflammation from the Inside Out
Through Claudia’s Concept, I’ve helped clients understand that weight loss isn’t just about calorie counting—it starts with gut healing. We look at inflammation as a cue, not a curse. By reprogramming your diet with anti-inflammatory, gut-supportive foods, you rewire your metabolism and give your body permission to release excess fat. The result? Real, sustainable transformation that starts in your microbiome and reflects in your mirror.
So here’s my challenge to you: examine your plate. Is it fighting or fueling inflammation?
Gut-Brain Axis and Appetite Regulation: What Your Gut Is Telling Your Mind (and Waistline)
Have you ever wondered why you crave chocolate when you’re stressed or feel full and content after a satisfying meal? That’s your gut having a conversation with your brain. This bi-directional communication is powered by what’s known as the gut-brain axis, and understanding it is key to unlocking stubborn weight issues.
The Gut and Brain: Not Just Pen Pals—Lifelong Best Friends
The gut and the brain are connected by a direct line of communication via the vagus nerve, a major pathway that allows these two organs to send chemical and electrical messages back and forth. Messages from your digestive tract can signal hunger, fullness, discomfort, or even emotion—and in turn your brain can influence your digestion and metabolism.
Interestingly, up to 90% of serotonin (your “feel-good” neurotransmitter) is actually produced in the gut. That means your emotional state is intrinsically linked to your gut environment. When working with clients at Claudia’s Concept, I often see how mood and digestion go hand-in-hand, and how improving one will instantly uplift the other.
Microbial Matchmakers: How Gut Bacteria Dictate Your Hunger
Your gut microbiota does more than just help digest food—it actively participates in regulating your appetite. Certain strains of bacteria stimulate the production of hormones like peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), both of which signal satiety to the brain. In simple terms, they tell you when you’ve had enough to eat.
- Lactobacillus and Bifidobacterium have been researched for their ability to promote satiety hormone release.
- One 2015 study published in the Nature Reviews Endocrinology journal highlighted that individuals with diverse gut flora had better regulation of GLP-1 and were less prone to overeating.
- Microbial fermentation of dietary fiber produces short-chain fatty acids (SCFAs) like butyrate, which further supports hormone balance and appetite control.
When Cravings Take Over: Microbiome Imbalance and Overeating
Now, here’s the catch. When your gut microbiome is out of balance—what researchers call dysbiosis—the conversation between your gut and brain becomes distorted. Harmful bacteria can manipulate your food preferences, leading to unhealthy cravings for sugar and processed fats. This isn’t about willpower; it’s about microbial influence.
A 2016 study in the journal Cell Metabolism demonstrated that dysbiotic guts tended to favor bacteria that fuel compulsive eating behavior by overstimulating the brain’s reward pathways. So, when your gut is off, your cravings aren’t just psychological—they’re microbial.
Stress, Anxiety, and the Emotional Gut Loop
Let’s talk about emotional eating. Stress triggers a cascade of hormonal responses, particularly increasing cortisol levels, which affect both microbiota composition and appetite regulation. Chronic stress has been shown to reduce beneficial bacteria and increase gut permeability, often referred to as “leaky gut.”
This is where I remind all my clients at Claudia’s Concept: nurturing your gut is not just about food—it’s about your emotional landscape too. A stressed brain can lead to an inflamed gut, which in turn disrupts hunger signals, increases cravings, and contributes to emotional eating cycles. One feeds into the other, quite literally.
So, Who’s Really in Charge—Your Head or Your Gut?
That’s the million-dollar question. And increasingly, science is pointing to a shared control system. This mutual relationship between gut health and brain signals creates a loop where the condition of one directly influences the other—and your weight sits right in the middle of that conversation. When the communication flows efficiently, you regain appetite control, reduce overeating, and enhance overall well-being.
At Claudia’s Concept, we use this knowledge to personalise nutrition strategies that empower you to create harmony between your gut and mind—because aligning both is the key to lasting weight control and vibrant health.
The Role of Dietary Fiber: Feeding the Gut and Controlling Weight
Let’s unravel one of the most underrated allies in your weight management journey—dietary fiber. Many people focus solely on calories, overlooking how profoundly fiber impacts gut health and, by extension, the number on the scale. But once you understand how fiber fuels your gut microbiome and supports sustainable weight control, your meals will never look the same again.
How Fiber Fuels Digestion and Microbial Diversity
Fiber doesn’t just keep you “regular.” It plays an essential role in nurturing the beneficial bacteria residing in your gut. These microbes ferment certain types of fibers (also called prebiotics) to produce short-chain fatty acids (SCFAs) such as butyrate, acetate, and propionate—compounds that actively preserve gut lining, reduce inflammation, and even influence metabolism.
Research published in Nature found that individuals consuming high-fiber diets had greater microbial diversity, which correlates directly with improved metabolic health and reduced weight gain. This microbial ecosystem thrives best when regularly fed diverse forms of fiber, which is the principle behind many of the meal plans I curate at Claudia’s Concept.
Soluble vs. Insoluble Fiber: Know Your Types
- Soluble fiber dissolves in water to form a gel-like substance. Found in oats, apples, flaxseeds, and legumes, it slows digestion and stabilizes blood glucose levels.
- Insoluble fiber does not dissolve but adds bulk to stool, promoting smoother bowel movements. It’s present in vegetables, whole grains, and wheat bran.
Although both types offer unique advantages, the real magic happens when they’re combined in your daily meals. Soluble fiber, in particular, serves as a fermented food source for gut microbes, leading to increased SCFA production—a proven contributor to fat oxidation and appetite reduction.
Fiber’s Role in Weight Regulation
Now, let’s talk about why fiber is non-negotiable for keeping your weight in check. Fiber-rich foods have a low energy density, meaning they provide fewer calories per gram. This allows you to eat satisfying portions without calorie overload. But there’s more.
Promoting Fullness, One Bite at a Time
High-fiber meals stimulate the release of satiety hormones such as peptide YY (PYY) and glucagon-like peptide-1 (GLP-1). These hormones signal to your brain that you’re full, reducing the drive to snack unnecessarily. In controlled trials, increased fiber consumption led to a decrease in overall caloric intake without a conscious effort to restrict food.
Slowing Digestion to Curb Overeating
Because fiber takes time to break down, it slows the gastric emptying process. This means food stays in your stomach longer, giving you a longer window of satiety. In fact, a 2015 study in the Journal of Nutrition observed that participants who consumed 30 grams of fiber daily lost significant weight—even when no other dietary changes were made.
Meals built on the pillars of Claudia’s Concept prioritize this reliable mechanism. Why? Because it’s not just about eating less—it’s about eating smarter, nourishing your microbiome, and allowing your body’s internal chemistry to work in your favor.
So next time you’re planning a meal, ask yourself a game-changing question: “Where’s the fiber?” The answer could directly influence your gut health and accelerate your weight goals.
Antibiotics and Gut Flora: A Delicate Balance
Have you ever taken antibiotics and noticed your digestion taking a turn for the worse? Or perhaps your weight began shifting in unexpected ways shortly after a course of medication? This isn’t coincidental. The relationship between antibiotics and your gut flora is far more intricate—and impactful—than most people imagine. Let me walk you through why maintaining the balance of your gut microbiome is essential, especially when antibiotics come into play.
How Antibiotics Disturb the Microbiome
Antibiotics are powerful tools against bacterial infections. They work by killing or inhibiting bacteria, but here’s the catch—they often can’t distinguish between the harmful pathogens causing illness and the beneficial bacteria that support healthy gut function. This indiscriminate action disrupts the delicate ecosystem within your gut, often with long-lasting consequences.
A landmark study published in the journal Nature Microbiology in 2016 found that even a single course of antibiotics could significantly alter gut microbial diversity for months. Yes—months. That’s enough time for metabolic shifts to occur, leading to changes in how your body stores fat, regulates appetite, and absorbs nutrients.
Reduction in Microbial Diversity
One of the most concerning impacts of antibiotics is the reduction in microbial diversity. Think of your gut microbiome as a rainforest teeming with various species, each playing a unique role in overall wellness. Antibiotics, especially broad-spectrum types, can slash this diversity by decimating entire microbial groups.
This drop in diversity weakens your gut’s resilience. With fewer beneficial microbes, harmful bacteria or yeast can overpopulate. Studies from the Human Microbiome Project have shown that lower microbial diversity correlates with a higher BMI, insulin resistance, and systemic inflammation—all major contributors to unwanted weight gain.
Increased Risk of Weight Gain and Digestive Problems
Yes, your antibiotics might be making you gain weight. Research conducted at the NYU Langone Medical Center found that repeated antibiotic use, especially in childhood, is linked to increased body weight and altered metabolism in adulthood. While the reasons are multifactorial, one key driver is the disruption of the microbial communities that regulate energy extraction from food and fat storage.
Moreover, digestive issues like bloating, constipation, or irregular bowel movements often arise after antibiotic therapy due to the imbalance in gut flora. This digestive shake-up can lead to increased cravings, unstable blood sugar levels, and ultimately, poor dietary choices—all of which sabotage your weight goals.
Tips for Restoring Gut Health After Antibiotic Use
The good news? Your gut is incredibly resilient. With the right strategies, you can nurse your microbiome back to health and re-establish the balance that supports fat loss and metabolic vitality. At Claudia’s Concept, I always focus on science-backed methods to reset the gut after antibiotic use.
- Probiotic Supplementation: Choose clinically studied strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii, which have been shown to restore gut flora and reduce antibiotic-associated diarrhea.
- Fermented Foods: Add plain yogurt, kefir, kimchi, and sauerkraut to your daily meals. These are rich in live cultures that repopulate your gut with beneficial bacteria.
- High-Fiber Diet: Focus on prebiotic fibers found in garlic, onions, asparagus, and chicory root. They feed the good bacteria, helping them flourish post-antibiotics.
- Timed Recovery: Give your gut a few weeks post-antibiotics to stabilize, gradually introducing probiotics and fiber within the first few days.
Restoring your gut is not just about avoiding digestive discomfort—it’s about resetting your entire metabolic balance. With the guidance from Claudia’s Concept and a targeted nutritional approach, your microbiome can return stronger and more diverse, putting you back in charge of your weight and wellness.
Leaky Gut Syndrome: A Leaky Future for Your Waistline?
Have you ever felt bloated, fatigued, and stuck with stubborn weight no matter how clean you’re eating? If so, your gut lining might be part of the problem. Let’s explore how a condition known as “leaky gut”—or increased intestinal permeability—can sabotage your weight and overall health.
What is Leaky Gut?
Your intestinal lining does more than just help absorb nutrients; it acts as a highly selective barrier. Think of it as a security system—allowing the good stuff like vitamins, minerals, and amino acids to pass through, while keeping out harmful invaders such as toxins, pathogens, and undigested food particles.
When this barrier becomes “leaky,” undigested proteins, endotoxins, and antigens seep into the bloodstream. What follows is a cascade of inflammation and immune activation—and this is where your waistline comes into play.
How a Compromised Gut Leads to Systemic Inflammation and Weight Gain
The human gut comprises over 4,000 square feet of epithelial lining. When this lining loses its integrity, endotoxins like lipopolysaccharides (LPS) escape into the bloodstream, triggering an immune response. Studies, including one published in the Journal of Obesity, have shown that elevated LPS levels are directly linked to increased body fat and insulin resistance.
Furthermore, leaky gut can disrupt hormones involved in hunger and metabolism. For example, inflammation driven by gut permeability can blunt leptin sensitivity—the hormone responsible for telling your brain you’re full. The result? Constant hunger and unexplained cravings, especially for sugar and processed carbs.
Deeper Metabolic Disruptions
Beyond hormones, a leaky gut alters how your cells use energy. Chronic low-grade inflammation, a direct outcome of intestinal barrier dysfunction, pushes the body into survival mode. This shifts metabolic processes toward fat storage rather than fat burning. Even worse, your body’s cortisol levels may rise in response, which increases abdominal fat deposition.
Science supports this mechanism. A 2017 meta-analysis in Frontiers in Immunology emphasized how elevated gut permeability correlates with metabolic disorders such as obesity, type 2 diabetes, and non-alcoholic fatty liver disease—all roadblocks to a healthy body composition.
Diet and Lifestyle: Healing a Leaky Gut
The good news is you can rebuild your gut lining and reverse these metabolic shifts. At Claudia’s Concept, we design personalized protocols that focus on gut repair through anti-inflammatory nutrition, mindful movement, and targeted supplementation.
- Eliminate inflammatory triggers: Gluten, refined sugars, processed oils, and excess alcohol are common culprits in increasing permeability.
- Load up on gut sealers: Bone broth, zinc, L-glutamine, and omega-3-rich foods like flaxseeds and wild fish support mucosal repair.
- Boost your fiber: Soluble fiber from flax, chia seeds, and oats nourishes the gut lining and promotes beneficial bacterial balance.
- Prioritize restorative habits: Deep sleep, breathwork, and stress management lower cortisol and allow the gut lining to regenerate.
When your gut lining is restored and your inflammatory markers fall, weight loss becomes intuitive—not a battle. Hormones regulate more effectively, hunger cues normalize, and your metabolism finds its natural, balanced rhythm.
If you’re trying everything and still not losing weight, your gut may be screaming for attention. At Claudia’s Concept, we don’t just guess—we assess. Healing begins when we turn our focus inward, starting with the gut.
How to Start Improving Your Gut for Better Weight Control
Ready to take charge of your weight by nurturing your gut? This stage is where transformation truly begins. You’ve already learned how gut health influences everything from digestion to hormones to inflammation. Now it’s time to put it into action—practically and effectively. At Claudia’s Concept, we don’t believe in crash diets or shortcuts. We rely on evidence-based habits that support a thriving microbiome, which in turn supports sustainable weight control.
Reduce Processed Foods and Added Sugars
Let’s start with what not to eat. Highly processed foods and refined sugars are the microbiome’s worst enemies. They promote dysbiosis—that’s when harmful bacteria outnumber the beneficial ones. This imbalance not only disrupts digestion but also leads to increased fat storage, cravings, and low-grade inflammation. A 2017 study published in Cell Metabolism found that mice fed a high-sugar, high-fat diet had measurably reduced microbial diversity and gained more weight than those on a whole-food diet—even when their caloric intake was the same.
Cutting back isn’t about deprivation. It’s about making smarter swaps: choose steel-cut oats over sugary cereals, opt for olive oil instead of processed dressings, and replace soda with sparkling water infused with citrus or herbs.
Increase Intake of Fiber-Rich Fruits, Vegetables, and Whole Grains
Now let’s talk about what your good gut bacteria thrive on: dietary fiber. And not just any fiber—varied sources matter. The human genome doesn’t digest fiber, but your bacteria do. When they ferment soluble fiber, they produce short-chain fatty acids (SCFAs) like butyrate, which support fat metabolism and appetite regulation. A 2019 report in the journal Nature Reviews Gastroenterology & Hepatology explained how SCFAs also improve insulin sensitivity and reduce inflammation, directly impacting weight control.
- Leafy greens like spinach and kale provide insoluble fiber for motility.
- Berries, apples, and pears offer soluble fiber and polyphenols to feed beneficial strains.
- Ancient grains—think quinoa, farro, and barley—deliver resistant starch, which feeds gut bacteria deep in the colon.
At Claudia’s Concept, we design fiber-forward meal plans that nurture a diverse microbial ecosystem, one plate at a time.
Incorporate Fermented Foods and Probiotics
Your microbiome isn’t just shaped by the food you feed it; you can also add new, beneficial species directly. Fermented foods are natural sources of probiotics—live microorganisms that restore balance. Yogurt with active cultures, kefir, tempeh, kimchi, kombucha, and fresh sauerkraut all introduce species like Lactobacillus and Bifidobacterium, which are linked to lower abdominal fat and improved insulin response.
Clinical trials like the 2020 double-blind study in Obesity Reviews have shown how daily probiotic supplementation can reduce BMI and fat percentage over a 12-week period. While probiotic supplements can be used selectively, naturally fermented foods provide not just bacteria but also enzymes and bioactive compounds that benefit gut health holistically.
Manage Stress Through Sleep, Mindfulness, and Physical Activity
Here’s the twist: your microbes don’t just respond to what you eat. They listen to how you live. Chronic stress, poor sleep, and sedentary routines disrupt gut barrier function and shift microbial populations in a direction that supports weight gain.
Mindfulness practices like yoga and meditation have been shown to modify gut-brain communication, lowering cortisol and systemic inflammation. In fact, a study from 2021 in the journal Psychoneuroendocrinology tracked improved microbiome balance and reduced visceral fat in individuals who regularly practiced mindfulness meditation.
Quality sleep—aiming for 7 to 9 hours—allows your gut lining to repair and regenerate, while regular exercise increases the abundance of microbes that contribute to lean body mass. It’s all connected, intricately and powerfully.
Avoid Unnecessary Antibiotic Use
Antibiotics are essential when used appropriately, but overuse strips the gut of its microbial defenses. Even a single course can reduce bacterial diversity for months. This reduction directly influences metabolic dysregulation and inflammation. According to a 2018 study in The BMJ, children who were administered antibiotics frequently in their first two years had significantly higher risk of childhood obesity.
Simple actions like opting for precise diagnostics before taking antibiotics, supporting microbial recovery post-treatment with probiotics, and choosing natural immune boosters can preserve microbial diversity—and let your gut continue doing what it’s uniquely designed to do: keep your metabolism on track.
Step by step, habit by habit, your gut becomes stronger and more balanced. It’s a central pillar of long-term weight control, and at Claudia’s Concept, we build every plan around it. Start with food, nurture with lifestyle, and let your body rise to its healthiest state—supported from the inside out.
Yes. Your gut microbiome influences how efficiently you digest food, absorb calories, regulate appetite hormones, and store fat—making it a key driver of body weight.
Differences in gut bacteria can affect how many calories are extracted from food. Some gut microbes harvest more energy, leading to easier fat storage.
An imbalanced gut can disrupt hunger hormones like GLP-1 and leptin, increase sugar cravings, and interfere with signals that tell your brain you’re full.
Fiber-rich vegetables, fruits, whole grains, legumes, fermented foods, and anti-inflammatory fats nourish beneficial bacteria and support a balanced microbiome.
Gut improvements can begin within a few weeks of consistent dietary and lifestyle changes, but sustainable weight regulation typically develops over several months.

