Weight Loss: Restrictive Dieting May Trigger Depression, Says New Study
In the pursuit of rapid weight loss, calorie restriction has become a popular strategy—especially among those seeking quick, visible results. Cutting calories seems like a logical solution to shedding pounds, and it’s often promoted as the foundation of most diet plans. But does eating less always lead to feeling better?
Recent scientific evidence is adding a critical layer to this conversation. A new study published in the Journal of Affective Disorders reveals a strong link between restrictive calorie intake and a heightened risk of developing depression. These findings challenge the assumption that fewer calories simply translate to better health, especially when mental well-being is on the line.
We’ll take a closer look at what this study uncovered, how restrictive eating patterns impact more than just body weight, and why your mood may suffer as much as your energy levels. Beyond the science, let’s explore smarter, healthier approaches to dieting that foster mental and emotional balance—not just numbers on a scale. Ready for a mindset shift?
Unpacking Calorie Restriction: What Happens When We Cut Too Much
What Does Calorie Restriction Really Mean?
When people talk about calorie restriction, they’re usually referring to a reduction in daily calorie intake, often below the recommended levels for maintaining body weight. It’s a common strategy used in weight loss programs—from commercial diets to self-imposed eating plans. The idea is simple: burn more than you consume, and the weight comes off.
For context, the average adult needs between 2,000–2,500 kcal per day, depending on age, sex, and activity level. Yet many popular weight loss plans recommend intakes as low as 1,200–1,500 kcal daily. That’s a 40–50% drop in energy input, a reduction that nudges the body into a survival-oriented state over time.
Why So Many People Turn to Low-Calorie Diets
People pursue calorie restriction for various reasons—some want quick results before an event, while others are influenced by social media trends or the promise of long-term health benefits. For others, it’s not even about aesthetics; managing a medical condition like high blood pressure or type 2 diabetes often begins with dropping weight. In each scenario, eating less is presented as not only effective but necessary.
How the Body Reacts to Low-Calorie Intake
Once calorie intake drops significantly, the body switches into conservation mode. Metabolically, things begin to shift. Resting metabolic rate (RMR)—the energy your body uses to maintain basic functions—starts to decrease. A study published in the journal Obesity (2012) showed that individuals following a calorie-restricted diet for 6 months experienced a measurable reduction in RMR, sometimes beyond what weight loss alone would predict.
Leptin and ghrelin, the hormones responsible for satiety and hunger, also start misfiring. Leptin drops, which decreases the sense of fullness, while ghrelin rises, stimulating appetite. The result? A constant feeling of hunger, often paired with fatigue, decreased performance, and mood instability.
Restrictive Dieting: A Modern Cultural Norm
Over the past two decades, restrictive dieting has woven itself into cultural narratives around beauty, success, and control. Not only do overweight individuals feel pressured to eat less, but even those at a healthy or underweight BMI often engage in chronic calorie restriction.
A cross-sectional study from the CDC’s National Health and Nutrition Examination Survey (NHANES) revealed that over 40% of normal-weight women aged 18–35 had engaged in caloric restriction in the past year. This isn’t confined to those seeking medical guidance—many are self-directed efforts driven by societal ideals and digital influencers who equate discipline with low-calorie eating.
This widespread belief that less is always better creates a dangerous blind spot: the physiological and psychological toll of constant under-fueling, which we’ll explore in the next section.
New Research Links Calorie Restriction to Depression—Here’s What You Need to Know
A Groundbreaking Study Sheds Light on the Hidden Costs of Dieting
In 2023, a peer-reviewed study published in the journal Obesity presented striking evidence: severe calorie restriction is strongly associated with increased symptoms of depression. Researchers followed over 1,900 adults across three clinical trial phases lasting six months to two years. Participants who engaged in aggressive calorie-cutting—defined as consuming 25% or more below their estimated daily energy requirements—reported higher levels of anxiety, lack of motivation, sadness, and sleep disturbances compared to those who adopted more moderate dietary changes.
These results didn’t emerge in isolation. Brain imaging conducted during the study showed reduced activity in the prefrontal cortex—an area crucial for decision-making, mood regulation, and impulse control. Simultaneously, participants showed disruptions in the balance of two critical neurotransmitters: serotonin and dopamine. Both play a central role in mood stability. When their synthesis declines, depressive symptoms can emerge rapidly.
What the Science Says About Your Brain on Low Calories
When the body is deprived of sufficient calories, it triggers a cascade of biochemical stress responses. Cortisol levels rise. The production of tryptophan—the amino acid precursor to serotonin—decreases. Glucose, the brain’s primary fuel, drops to suboptimal levels. These shifts don’t just affect energy; they alter mood, emotional reactivity, and even memory formation.
Dr. Anja K. Papenbrock, lead researcher on the study, emphasized this link: “Calorie intake directly affects neural circuits, particularly those that control emotion. We observed cognitive sluggishness, heightened emotional sensitivity, and impaired stress resilience among participants with the strictest diets.”
Who’s Most Vulnerable to These Effects?
- Individuals with a history of depression or anxiety: Caloric restriction lowered their stress threshold significantly, increasing relapse risk.
- Teenagers and young adults: During developmental years, energy needs are higher. Restrictive diets appeared to impair executive function and heighten irritability.
- Frequent or chronic dieters: For those who’ve engaged in years of yo-yo dieting, serotonin pathways may already be weakened, making them highly reactive to small physiological changes.
Why does this matter? Because the pursuit of thinness often overshadows the body’s psychological needs. Many dieting regimens ignore mood as a metric of health. But this study makes one thing clear—how you eat directly influences how you feel.
Consider this: are your low-calorie goals supporting your mental clarity, or sabotaging it?
The Diet and Mood Connection
Ever noticed how your mood shifts when you’re following a strict diet? That’s not your imagination—it’s the chemistry of your brain reacting to what you’re putting (or not putting) into your body. The relationship between diet and emotional well-being runs deeper than most people realize, and researchers have been tracing these connections with growing precision.
How What You Eat Shapes How You Feel
The foods you consume directly influence neurotransmitter activity, hormonal balance, and brain function. Nutrients act as precursors for mood-regulating chemicals—essentially, they become the raw materials for your brain’s emotional toolkit. When calorie intake decreases drastically, the body begins to ration nutrients, prioritizing survival over mood balance.
This shift doesn’t go unnoticed by the brain. Emotional sensitivity, irritability, and low energy can surface quickly, especially when nutrient reserves are depleted. Food isn’t just fuel—it’s information. And when that information signals “famine,” cognitive and emotional function start to suffer.
Essential Nutrients: The Mood-Stabilising Allies
Let’s break down a few key nutrients that are vital for mood regulation and how calorie restriction might be interfering with them:
- B-vitamins: Vitamins B6, B9 (folate), and B12 are crucial for the synthesis of neurotransmitters like serotonin and dopamine. A deficiency in these vitamins has been linked to higher rates of depression and mental fatigue. Without adequate intake—common in low-calorie diets—the brain struggles to maintain emotional equilibrium.
- Omega-3 fatty acids: These polyunsaturated fats, particularly EPA and DHA found in fatty fish, reduce inflammation in the brain and support neuronal flexibility. Clinical trials have consistently shown an association between low omega-3 intake and depressive symptoms, especially in those with dietary fat restrictions.
- Iron: Iron plays a major role in oxygen delivery to the brain and the production of dopamine, a neurotransmitter tied to motivation and pleasure. Women on calorie-restricted diets are particularly vulnerable to iron deficiency, which can contribute to cognitive dullness and low moods.
Serotonin, Calories, and the Brain’s Reward System
Serotonin—the body’s natural mood stabilizer—is heavily dependent on both dietary input and energy availability. It’s synthesized from the amino acid tryptophan, which competes with other amino acids to cross the blood-brain barrier. Here’s the catch: tryptophan uptake increases when carbohydrate intake is adequate. On calorie-restricted plans, especially those that limit carbs, serotonin production diminishes.
Additionally, under conditions of caloric scarcity, the brain initiates stress responses through the hypothalamic-pituitary-adrenal (HPA) axis. The result? Elevated cortisol levels and reduced serotonin activity—an environment strongly linked to anxiety, irritability, and depression.
Ask yourself this: is the hunger worth the emotional toll? The brain interprets food scarcity as a threat. It pulls resources from emotional regulation systems to safeguard basic survival. That’s biology at work, not a lack of self-control or motivation.
Feeding your brain isn’t indulgent—it’s essential. Balance and variety in your diet help create biochemical harmony, which lays the foundation for stable mood and mental clarity. Next time you measure your portion sizes, ask: is my brain getting fed too?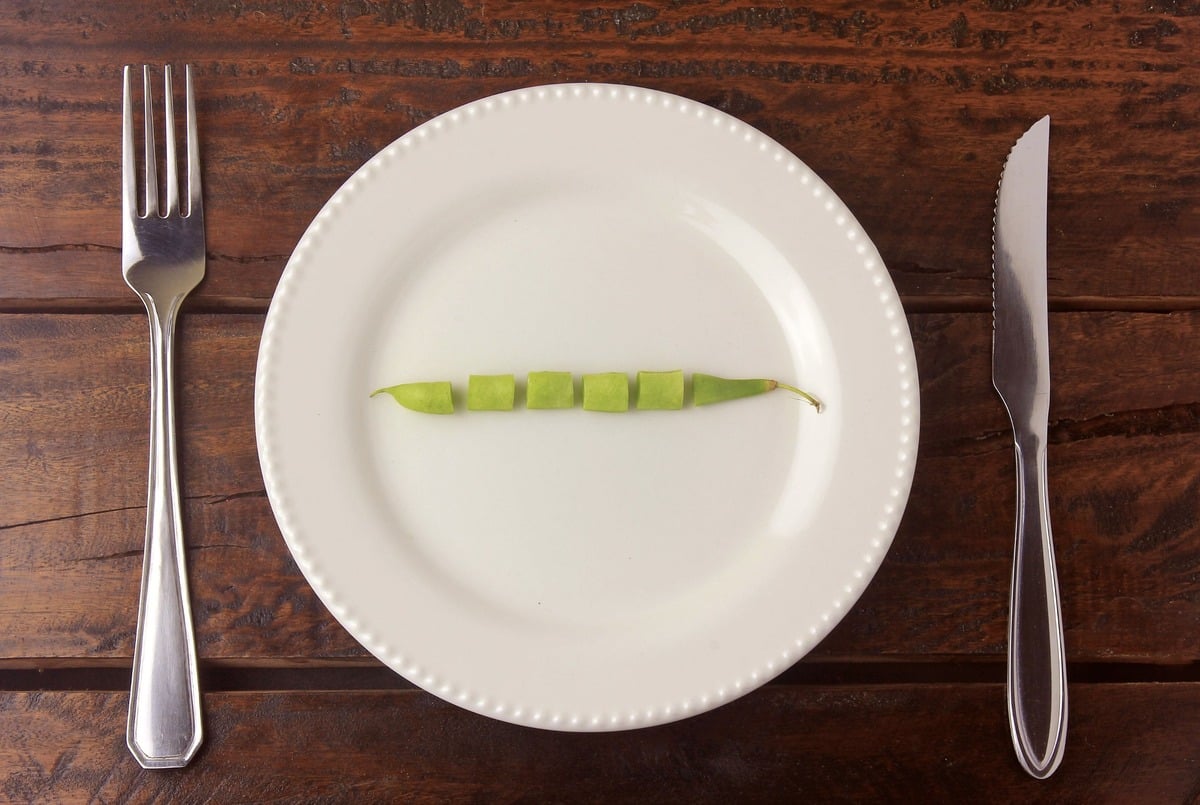
Why Low-Calorie Diets Can Drain Your Nutrients—and Your Mood
The Nutrient Cost of Cutting Calories
While calorie restriction is often marketed as the golden ticket to weight loss, strategic cutting quickly unravels when essential nutrients are lost along the way. Diets that severely restrict calorie intake also tend to limit foods rich in minerals and vitamins crucial for brain function and emotional stability. Over time, this creates an invisible deficiency burden that directly impacts your energy, focus, and mood.
The Commonly Missed Micronutrients
When calorie consumption dips below your body’s basic needs, several nutrients fall through the cracks. Among the most frequently deficient are:
- Iron – Essential for transporting oxygen in the blood, low iron levels contribute to fatigue, difficulty concentrating, and increased irritability.
- Magnesium – Involved in over 300 enzymatic reactions, magnesium influences nerve transmission and mood regulation. A deficiency here often shows up as anxiety, sleep disturbances, and low energy.
- Zinc – This trace mineral is vital for neuroplasticity and neurotransmitter release. Inadequate intake impairs cognitive performance and has been directly linked to symptoms of depression.
- Folate (Vitamin B9) – Crucial for cell growth and the production of serotonin and dopamine. Deficiency in folate is strongly associated with depressive symptoms and low emotional resilience.
Recognising the Subtle Signs of Deficiency
Not all deficiencies scream their presence with obvious symptoms. Instead, they quietly erode well-being. Think about those foggy mornings where thoughts arrive slowly, or the sudden mood swings you chalk up to stress. These could be indicators that your body isn’t getting enough of the right nutrients.
Look for persistent signs such as:
- Chronic fatigue, even after a full night’s sleep
- Irritability or heightened emotional sensitivity
- Memory lapses or difficulty concentrating
- Poor stress tolerance
The Nutrient-Mood Link, Backed by Science
The relationship between nutritional status and psychological well-being is well-established in clinical nutrition research. For instance, a meta-analysis published in Psychiatry Research (2017) reviewed studies on micronutrient status and depression, concluding that low levels of magnesium, zinc, and folate were significantly associated with increased depressive symptoms. In another 2020 study in the International Journal of Environmental Research and Public Health, participants with lower serum iron were more likely to experience mood disorders and had slower cognitive processing.
When dietary intake is insufficient—especially in long-term calorie-restricted plans—the brain doesn’t receive the raw materials it needs to synthesise neurotransmitters like serotonin and dopamine. Without them, emotional stability crumbles. What starts as ‘just a diet’ can quickly manifest as persistent sadness, social withdrawal, and mental fatigue.
Reflection Time
Ask yourself this: is the number on the scale worth the daily trade-off in vitality, mood clarity, and emotional equilibrium? The nutrients we eat feed more than just our physical structure—they shape how we think, feel, and cope.
What Prolonged Dieting Does to Your Body and Mind
Cutting calories may seem like a logical step towards your weight loss goals, but have you ever wondered what happens beneath the surface—metabolically and psychologically—when you stay in a calorie deficit for too long?
Metabolic Slowdown: The Body’s Energy-Saving Mode
The human body is remarkably adaptive. Prolonged calorie restriction sends a signal that energy is scarce, triggering a series of protective metabolic changes. One significant change involves a reduction in basal metabolic rate (BMR). In a study published in Obesity Research, individuals involved in long-term calorie restriction showed a reduction in metabolic rate that persisted even six years after initial weight loss. Simply put: the body learns to do more with less energy, burning fewer calories even at rest.
Hormonal shifts accompany this metabolic slowdown. Leptin—often called the satiety hormone—takes a notable hit. Low leptin levels increase hunger and can trigger overeating, making weight maintenance harder. At the same time, levels of ghrelin, the “hunger hormone,” rise, nudging you to eat more. Thyroid hormones, particularly triiodothyronine (T3), also decrease, further contributing to reduced metabolic efficiency and feelings of lethargy.
How Dieting Affects Mental Health
Now shift your focus to the psychological terrain. When you’re constantly monitoring calories, food can become a source of anxiety rather than nourishment. Chronic dieting has been linked to elevated cortisol levels—the body’s primary stress hormone. High cortisol doesn’t just increase emotional sensitivity; it also contributes to fat storage around the abdomen and impairs sleep quality, making the overall weight loss process more emotionally taxing.
There’s also the creeping effect of disordered thoughts around food. What begins as a structured eating plan can spiral into obsessive behaviors: measuring every bite, avoiding social situations involving meals, and experiencing guilt after eating. A 2013 study in the International Journal of Eating Disorders found that restrained eaters showed increased vulnerability to binge episodes when under stress, illustrating the fine line between dieting and disordered eating.
The Yo-Yo Dieting Cycle and Long-Term Mood Consequences
Each cycle of weight loss and regain—commonly known as yo-yo dieting—disrupts not just your metabolism, but also your emotional equilibrium. Researchers at the University of California, Los Angeles conducted a meta-analysis and found that over two-thirds of dieters regain more weight than they initially lost. But the emotional toll often goes unmeasured—fluctuating weight is associated with increased feelings of failure, body dissatisfaction, and even depression.
What’s more, long-term psychological distress accumulates with each failed diet attempt. The constant dieting mindset undermines self-efficacy and self-worth. It’s not just about willpower—it’s about physiology working against you, and a cultural pressure to shrink your body overriding signals from your mind.
So, instead of asking “Why can’t I stick to the diet?” consider a different angle: “What if the diet is working against my body and mental health?”
Recognising the Signs of Diet-Induced Depression
Cutting calories may seem like a logical step toward weight loss, but when it leads to emotional strain, your body is sending a clear message. The psychological costs of under-eating are often underestimated. How can you tell if your diet is no longer supporting your well-being? Let’s explore the core indicators—both emotional and physical—that you shouldn’t ignore.
Emotional and Physical Warning Signs
Diet-induced depression doesn’t always look the same as other forms of depression. Its symptoms often surface slowly, quietly tied to nutrient deprivation and psychological stress related to food. Here’s what to watch for:
- Persistently low mood, even when weight is improving: If you find yourself feeling sad or emotionally flat most days, despite achieving weight loss goals, this could point to a deeper nutritional or psychological imbalance.
- Loss of interest in food and pleasure: Enjoyment of meals tends to vanish in the face of strict restriction. When even your favorite dishes no longer appeal to you and you eat only for function, that’s a red flag.
- Chronic fatigue, disrupted sleep, and fuzzy focus: Glucose is the brain’s primary energy source. A consistent calorie deficit can leave you drained, mentally sluggish, and restless at night. Research published in the journal Appetite (2018) reported that women on low-energy diets experienced significantly more fatigue and lower cognitive performance than those on balanced nutrition plans.
- Withdrawing from people and increased irritability: If you’re isolating yourself socially or reacting more sharply to everyday interactions, these behaviors may signal a deeper mental health shift fueled by dietary imbalance.
When to Seek Support
You don’t need to hit a crisis point to seek help. In fact, the earlier you respond, the easier it is to reverse course. Here’s how support structures can step in:
- Counseling or psychotherapy: Talking to a mental health professional can help uncover the emotional roots behind restrictive patterns and offer coping strategies that don’t rely on food control.
- Nutritional evaluation: A qualified nutritionist can assess whether you’re meeting your body’s needs for essential nutrients—especially B vitamins, iron, tryptophan, and omega-3 fatty acids, which are all deeply connected to mood regulation.
- Medical consultation: Hormonal shifts, thyroid imbalances, or clinical depression can develop or worsen with long-term calorie restriction. Consulting your healthcare provider ensures that both physical and mental health are properly evaluated.
Long-term happiness and health don’t come from hunger. If your diet leaves your spirit depleted, it’s time to listen inward and consider a new approach.
Rethinking Health: Where Nutrition Meets Mental Wellbeing
Redefining what it means to be truly healthy starts with shifting our focus—not just from weight management, but toward nurturing both the body and the mind. It’s not just about the number on the scale. Nutrition plays a crucial role in shaping our mental landscape, and integrating this awareness can transform how we approach eating habits, body image, and long-term wellness.
Eating Patterns That Support Mental Wellness
Certain dietary patterns consistently show strong associations with better mental health outcomes. The Mediterranean diet, rich in fruits, vegetables, whole grains, fish, nuts, and olive oil, has been extensively studied for its protective effect against depression.
- The SMILES trial (2017) demonstrated that adults with major depressive disorder experienced significant mood improvements after following a Mediterranean-style eating pattern for 12 weeks. Notably, one-third of participants achieved full remission.
- Dietary fiber from whole plant foods increases production of short-chain fatty acids in the gut—substances that actively influence brain function through the gut-brain axis.
- Omega-3 fatty acids, found abundantly in fatty fish, support neurogenesis and regulate neurotransmitter activity. Their deficiency has been linked to higher rates of mood disorders.
Structure matters as much as food choices. Eating at regular intervals stabilizes blood glucose levels, which directly impacts mood and cognitive function. Skipping meals—especially breakfast—can lead to irritability, fatigue, and difficulty concentrating throughout the day.
A Collaborative Approach: Nutrition and Behavior Together
Long-term success comes from addressing more than what’s on your plate. Integrating the expertise of registered dietitians and behavioral therapists allows for a more complete and sustainable journey toward health. This multidisciplinary model connects nutrition science with behavioral change principles, emotional resilience, and body image healing.
- Dietitians guide balanced eating plans tailored to individual needs, nourishing both the body and the brain.
- Behavioral therapists uncover subconscious patterns around food, emotional eating, self-worth, and perfectionism that can interfere with health goals.
- Together, they create realistic strategies to build lifelong habits aligned with psychological well-being.
In practice, this looks like meal structures that align with your social rhythms, mindset coaching around self-talk, and nutrition advice that acknowledges cultural preferences and emotional satisfaction.
Health Is More Than a Dress Size
The narrative that equates thinness with wellness continues to dominate modern culture; it’s time to replace it. Health is a complex tapestry, woven from physical vigor, emotional balance, social connection, and self-acceptance. A person eating nutrient-dense meals, moving joyfully, sleeping well, and thriving emotionally may not fit outdated body ideals—but their health is vibrant and real.
How would your approach to health change if the goal was to feel grounded, clear-headed, energized, and connected—instead of simply lighter? Rethinking our definition of “healthy” begins with asking better questions and measuring success in more meaningful terms.
Your Mental Health Deserves More Than a Calorie Count
Chasing weight loss through calorie restriction alone doesn’t just drain physical energy—it disrupts emotional balance, too. We’ve seen how reduced energy intake can lead to mood swings, impair cognitive function, and even trigger depressive symptoms, especially when nutritional needs aren’t being met.
If your body is sending distress signals—like fatigue, irritability, low motivation, or anxiety—don’t dismiss them as simply part of the diet process. These reactions are your mind and body asking for care, not more restriction.
Instead of focusing solely on numbers—on the scale or on a food label—shift your attention to how you feel. Are you energized in the morning? Does your mood remain stable throughout the day? Do you enjoy the meals you’re preparing and eating? These questions matter. In fact, they hold the key to sustainable, nourishing wellness.
Health will never be defined by calorie deficits alone. It’s a reflection of balance—of mindful eating, supportive habits, and emotional well-being. In every weight loss journey, your mental health doesn’t just play a supporting role—it shares the spotlight.
So as you pursue change, don’t sacrifice vitality for restriction. You deserve a plan that fuels both mind and body—because your emotional health is not expendable, and it certainly isn’t secondary.
Yes. Recent studies, including one published in the Journal of Affective Disorders, have found a strong link between restrictive dieting and increased symptoms of depression. Drastically reducing calorie intake can alter brain chemistry, lower serotonin and dopamine levels, and elevate cortisol, all of which contribute to mood instability and depressive symptoms.
Low-calorie diets deprive the body of essential nutrients like B-vitamins, iron, magnesium, and omega-3s, all of which are crucial for emotional regulation and brain function. Without enough of these nutrients, neurotransmitter production is impaired, which can lead to anxiety, fatigue, and depression.
People with a history of depression or anxiety, teenagers and young adults, and chronic dieters are particularly vulnerable. These groups may have increased sensitivity to nutritional imbalances and hormonal shifts caused by under-eating.
Yes. Instead of extreme calorie-cutting, focus on balanced, nutrient-rich diets like the Mediterranean diet, eat at regular intervals, and work with a qualified nutritionist and behavioral therapist to build sustainable habits that support both physical and mental well-being.
Warning signs include chronic fatigue, low mood, irritability, sleep issues, loss of interest in food or social activities, and difficulty concentrating. These may indicate that your current diet is too restrictive and lacking essential nutrients your brain needs to function optimally.

