H. Pylori Diet: The Best Foods to Eat and Avoid for a Healthier Gut
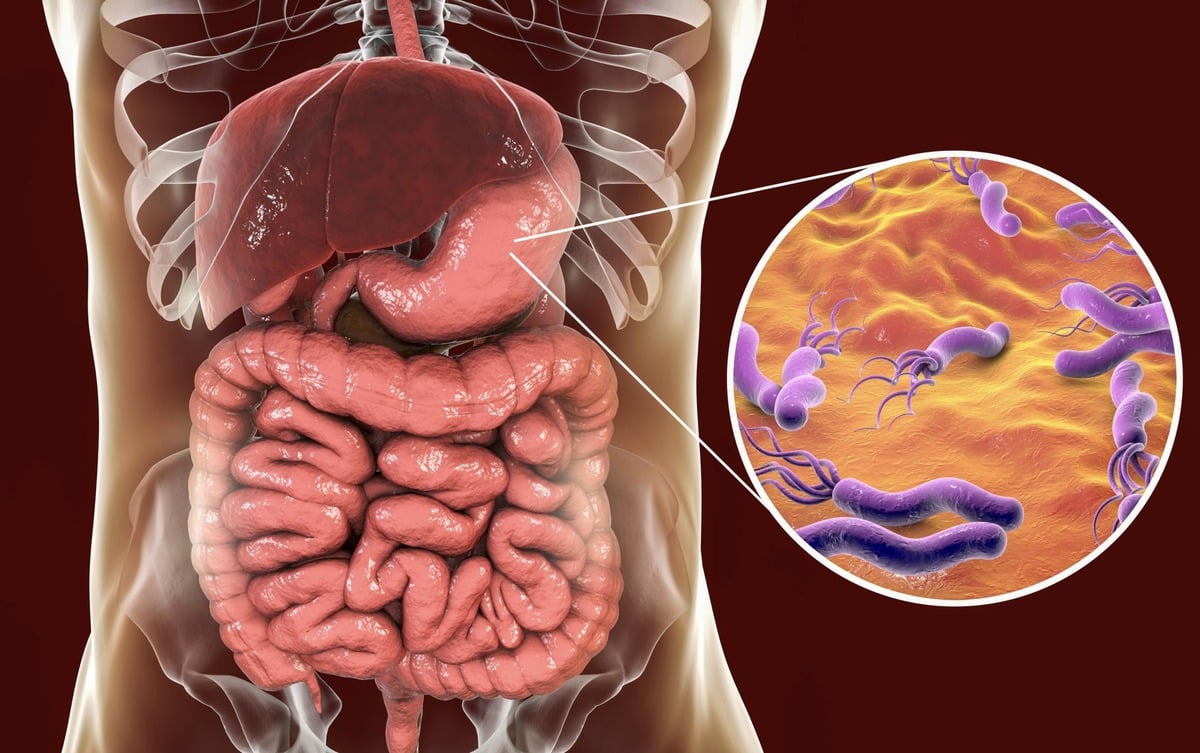
Helicobacter pylori—commonly called H. pylori—is a spiral-shaped bacterium that sets up camp in the stomach and upper part of the small intestine, often silently. It’s estimated that more than 50% of the global population carries this bacteria, though not all experience symptoms. When symptoms do surface, they can include persistent bloating, heartburn, nausea, unexplained weight loss, and in more serious cases, ulcers or gastritis.
What makes H. pylori particularly harmful is its ability to compromise the stomach lining—weakening the protective mucous barrier and increasing inflammation. This chronic irritation not only disrupts digestion but also hampers nutrient absorption. Over time, the imbalance it causes in gut microbiota can set off a chain reaction, affecting overall gut health and immune resilience.
Now here’s the good news: while antibiotics are often needed short-term, what you put on your plate daily has long-term power. The right diet can limit H. pylori’s growth, support healing of the gut lining, and strengthen your microbiome. At Claudia’s Concept, we focus on personalised food strategies that do exactly this—restore your gut’s natural defence while promoting total digestive wellness. Curious which foods help you fight back and which ones invite trouble? Let’s explore what your plate should (and shouldn’t) look like when you’re managing H. pylori.
Behind the Bacteria: Understanding H. Pylori Infection
What Causes an H. Pylori Infection?
You typically don’t feel it coming, but Helicobacter pylori, or H. pylori, has a stealthy way of invading the body. This spiral-shaped bacterium is mainly transmitted through contaminated food, water, or direct contact with saliva. That includes something as simple as sharing utensils or kissing. Inadequate sanitation and crowded living conditions increase the risk significantly, which is why it’s more prevalent in developing regions.
Once inside the digestive tract, this bacterium thrives in the harsh acidic environment of the stomach by producing an enzyme called urease. This enzyme breaks down urea into carbon dioxide and ammonia, which neutralizes stomach acid just around the bacteria—creating a protective cloud, so to speak. This evasion tactic allows it to survive and multiply while the rest of the stomach remains acidic.
How H. Pylori Triggers Complications Like Gastritis and Ulcers
When left unchecked, H. pylori sets off a chain of damage. It doesn’t just sit harmlessly—it disrupts the protective mucous layer of the stomach lining. This layer is designed to shield the tissue from stomach acid, but as H. pylori erodes it, the tissue becomes vulnerable to acid attacks. Imagine stripping away the roof of your home during a monsoon—damage is inevitable.
This damage prompts an immune response, leading to chronic low-grade inflammation known as gastritis. If the bacteria stay long enough, they dig deeper, literally and figuratively, leading to the formation of peptic ulcers. The World Health Organization reports that H. pylori is responsible for up to 90% of duodenal ulcers and 80% of gastric ulcers globally. That’s not a marginal impact—it’s a dominant cause.
The Bacteria’s Role in Damaging the Stomach Lining
The most dangerous part about H. pylori isn’t just its ability to survive. It’s the way it manipulates its environment. Apart from urease, the bacteria also secrete special proteins—like CagA and VacA—which infiltrate the lining cells and disrupt normal cellular functions. Studies published in Gut Microbes journal confirm that these proteins can even alter cell signaling and suppress immune defenses, delaying healing and worsening inflammation over time.
This persistent damage can evolve beyond ulcers. Long-standing infection with certain virulent strains of H. pylori is a significant contributor to gastric cancer development. That’s why handling the infection early—along with dietary and clinical interventions—is a non-negotiable strategy.
Why Treatment Alone Isn’t Enough—Diet Plays a Critical Role
While antibiotics and proton pump inhibitors can remove the immediate bacterial threat, recovery isn’t complete without support from your diet. The right food choices help repair the gastric lining, reduce inflammation, and strengthen the microbiome. That’s exactly where Claudia’s Concept comes in—to empower your gut healing through precise nutrition strategies tailored to support your body through—and beyond—infection.
In my clinical experience, patients who combine the prescribed medical treatment with a therapeutic diet recover faster and experience less recurrence. By recognizing food as functional medicine, we begin to restore the digestive lining and bring renewed vitality from the inside out.
Is Your Gut Trying to Tell You Something? Recognising the Signs and Symptoms of H. Pylori
If you’ve been experiencing off-and-on stomach discomfort, frequent bloating, or a strange pattern of unexplained weight loss—it’s time to listen. These aren’t just random symptoms. They could be your body signalling a Helicobacter pylori (H. pylori) infection. At Claudia’s Concept, gut health is at the centre of our nutrition philosophy, and identifying these signs early can drastically improve outcomes. Let’s break down the key symptoms to watch for and understand what your body might be trying to tell you.
Common Signs to Watch For
- pylori is a spiral-shaped bacterium that lives in the mucosal lining of the stomach. It can disrupt normal digestive processes, trigger inflammation, and, over time, cause damage that leads to chronic conditions. Let’s explore what symptoms often show up.
- Abdominal Pain or Soreness: This is often the earliest and most noticeable sign. Typically felt in the upper or middle part of your abdomen, the pain can be gnawing, burning, or aching. Many feel it more intensely when the stomach is empty. Research from the Mayo Clinic indicates that this type of discomfort is among the most reported symptoms — a direct result of inflammation caused by H. pylori colonisation.
- Bloating and Indigestion: After meals, do you frequently feel like your stomach is full or stretched beyond what’s normal? The bacterial imbalance caused by H. pylori disrupts enzyme activity and acid production, making it harder to break down food. This leads to bloating, gas, and discomfort — symptoms strongly supported by findings in the Journal of Digestive Diseases.
- Unexplained Weight Loss: Dropping kilos without changing your diet or workout routine might seem like a pleasant surprise—until it’s not. H. pylori often reduces appetite and impairs nutrient absorption. According to a 2021 study published in Gut Microbes, patients with chronic H. pylori infection showed measurable nutrient deficiencies, particularly in iron and vitamin B12, both linked to weight fluctuation.
- Frequent Burping and Nausea: Increased belching—especially between meals—isn’t just annoying. It can be a sign of trapped gas and disrupted digestion. Nausea may also accompany it, particularly in the mornings. These symptoms reflect altered stomach acidity and motility caused by the infection.
When to See a Doctor
Occasional bloating or indigestion happens to nearly everyone—but when these symptoms repeat consistently or interfere with daily life, that’s your cue for action. At Claudia’s Concept, we encourage people not to dismiss persistent discomfort as “normal.” If you notice a combination of the above symptoms persisting beyond a week, it’s time to talk to your healthcare provider. A simple breath, stool, or blood test can identify H. pylori, and from there, you can begin building a healing plan supported by nutrition.
Staying connected to your body’s cues is the first step. Know the signs, trust what you’re feeling, and take action. With the right diet, lifestyle tweaks, and guidance, managing H. pylori becomes completely achievable.
Conventional Treatments and Dietary Support for H. Pylori
When it comes to treating Helicobacter pylori, medical professionals typically rely on well-established protocols. But addressing the infection doesn’t stop with just prescriptions—dietary support plays a pivotal role in healing and recovery. Understanding how to sync your nutrition with your medical treatment can dramatically enhance results and reduce discomfort.
Common Drugs and Treatment Protocols
Let’s start with what’s commonly known as triple therapy. This frontline treatment includes:
- Two antibiotics, often amoxicillin and clarithromycin, which work to target the H. pylori bacteria directly.
- A proton pump inhibitor (PPI), such as omeprazole or lansoprazole, which reduces stomach acid, creating a more hostile environment for the bacteria and aiding the healing of the stomach lining.
Some patients may be prescribed quadruple therapy, which adds metronidazole and bismuth subsalicylate to the mix, especially in areas where antibiotic resistance is high.
This treatment typically spans 10 to 14 days and, when followed correctly, has a 70% to 85% eradication success rate. However, without proper diet and lifestyle integration, the efficacy—and tolerance—of these drugs can drop significantly.
Interaction Between Antibiotics and Food
During therapy, what you eat can influence how well the drugs work. Certain foods can interfere with antibiotic absorption or intensify side effects. For instance:
- Calcium-rich foods—like dairy—can reduce the body’s ability to absorb antibiotics such as tetracycline.
- Grapefruit and grapefruit juice can interfere with the metabolism of PPIs, altering their effectiveness.
- Alcohol, when mixed with metronidazole or tinidazole, can cause severe nausea and vomiting.
So, it’s not just about swallowing pills—it’s about creating a dietary environment that allows these drugs to do their job without added hurdles.
Why Diet Plays a Critical Role During Treatment
- pylori isn’t just a bacterial nuisance; it damages the stomach lining, disrupts acid production, and inflames the entire digestive environment. Antibiotics alone might clear the infection, but only an effective diet will rebuild, restore, and support your gut.
At Claudia’s Concept, I always emphasize that treating H. pylori is not just about elimination—it’s about restoration. A supportive diet accelerates mucosal healing, balances gut flora, reduces unwanted side effects, and strengthens immunity.
Supporting the Body Through Anti-Inflammatory and Healing Foods
While medications handle the bacteria, food handles the inflammation. In fact, research from the Journal of Clinical Gastroenterology (2015) shows that gut-friendly, polyphenol-rich foods have the power to reduce inflammation markers and improve treatment outcomes in H. pylori patients.
Here’s what I advise my clients to integrate during treatment:
- Cooked green vegetables like spinach and kale for vitamin K and antioxidants.
- Bone broth for its high collagen content which helps strengthen the gut lining.
- Fermented foods such as kimchi or sauerkraut that contain live cultures supporting microbiota balance—best consumed post-antibiotic course to aid recolonization.
- Omega-3 rich sources like flaxseeds and walnuts to suppress cytokine-driven inflammation.
Consistent choices like these align perfectly with the healing philosophy at Claudia’s Concept. They work synergistically with conventional therapy, not in opposition.
A question I often ask my clients during one-on-one sessions: If you’re asking your body to fight infection, are you also giving it the tools to rebuild? Because with the right foods, that answer is always yes.
The Best Foods to Eat with H. Pylori: Heal, Soothe, and Strengthen from Within
Managing H. pylori isn’t just about eliminating the bacteria—it’s about creating an environment where your digestive system can thrive. And that begins with what you put on your plate. The right foods don’t just soothe symptoms; they actively support healing, bolster the gut’s natural defences, and make life harder for H. pylori to survive. Let me show you what to focus on—at Claudia’s Concept, we prioritise foods that are nutrient-dense, science-supported, and naturally healing.
High-Antioxidant Foods: Rebuilding the Stomach Lining
- pylori damages the stomach lining, but antioxidants can help reverse the effect by reducing oxidative stress and encouraging tissue repair. Vibrant vegetables and fruits are your best allies here.
- Berries– Blueberries, raspberries, and strawberries are brimming with anthocyanins, which have proven gastroprotective activity. A 2019 study published in Biomedical and Pharmacology Journal demonstrated that berry polyphenols inhibit bacterial adhesion, including H. pylori.
- Leafy greens– Spinach, kale and Swiss chard provide essential vitamins like A and C, which support epithelial healing and immune function.
- Broccoli– Especially broccoli sprouts, which contain sulforaphane—a powerful compound shown in a study published in Cancer Prevention Research to suppress H. pylori colonisation in human gastric mucosa.
Anti-Inflammatory Superstars: Calming Inner Irritation
Inflammation fuels the progression of H. pylori-related gastritis. Anti-inflammatory foods reduce swelling, ease discomfort, and promote recovery. Incorporate these healing staples into your daily meals:
- Turmeric– Rich in curcumin, this golden root has been shown to suppress inflammatory pathways. Research in the World Journal of Gastroenterology reports curcumin reduces gastric inflammation caused by H. pylori.
- Ginger– Beyond its soothing qualities, ginger disrupts bacterial biofilms. Its active compounds, like gingerol, have intensive anti-inflammatory action.
- Salmon– A rich source of omega-3 fatty acids, which consistently lower systemic inflammation. EPA and DHA, the fatty acids in salmon, have also been shown to support mucosal immunity.
Probiotic-Rich Foods: Restoring Gut Harmony
- pylori disrupts gut flora, but probiotics rebuild balance. Clinical trials, such as those reviewed in a 2020 meta-analysis in Frontiers in Microbiology, confirm that probiotics not only alleviate digestive symptoms but also improve antibiotic treatment outcomes for H. pylori eradication.
- Yogurt– Look for live active cultures like Lactobacillus and Bifidobacterium.
- Kefir– A fermented milk that’s more potent in probiotics than yogurt, kefir also provides B-vitamins and beneficial yeasts.
- Miso & Sauerkraut– Fermented foods like miso (soy-based) and sauerkraut (cabbage-based) bring diverse strains of beneficial bacteria to the gut.
High-Fiber Choices: Feeding the Good Bacteria and Reducing Inflammation
Dietary fiber supports the growth of gut-friendly bacteria, regulates motility, and binds toxins. Soluble fiber, in particular, forms a soothing gel-like coating in the stomach.
- Oats– Rich in beta-glucan, which binds bile acids and helps maintain microbial balance.
- Legumes– Beans, lentils, and peas not only boost fiber intake but also provide resistant starch that ferments in the colon, producing healing short-chain fatty acids (SCFAs).
- Apples & Pears– These fruits supply pectin, a soluble fiber with prebiotic benefits and anti-inflammatory properties.
Soothing Staples: Gentle on the Stomach, Rich in Properties
Certain foods go beyond nutrition—they actually calm the digestive tract almost instantly. At Claudia’s Concept, I often recommend these when clients are experiencing acute symptoms.
- Bananas– Their natural antacid effect comes from their high mineral content, particularly potassium and magnesium. Bananas also help repair the stomach lining.
- Manuka Honey– This New Zealand gem has clinically verified antibacterial activity. A 2022 article in Clinical Microbiology Reviews highlights manuka’s methylglyoxal compound as effective against antibiotic-resistant strains of H. pylori.
- Green Tea– Loaded with polyphenols and catechins, green tea reduces inflammation while directly inhibiting H. pylori growth, according to in vitro research published in Applied Microbiology and Biotechnology.
Lean Proteins: Supporting Tissue Repair Without Strain
Protein is essential for cellular repair and immune responses. However, heavy or fatty cuts can irritate the gut. Lean sources are ideal.
- Skinless poultry– Turkey or chicken breast delivers a clean source of amino acids, without irritating fats.
- Tofu– A plant-based, easily digestible protein that supports muscle maintenance and gut equilibrium.
- Baked fish– White fish like cod or haddock offers low-fat protein with anti-inflammatory selenium and B12.
Healthy Fats: Healing with Balance
Contrary to outdated advice, certain fats promote healing when used wisely. The key is moderation and quality.
- Olive oil– Extra virgin olive oil is rich in polyphenols with anti-H. pylori activity, as shown in a 2012 Journal of Agricultural and Food Chemistry
- Avocados– Contain monounsaturated fats, fiber, and plant sterols—supportive of mucosal healing and nutrient absorption.
- Nuts– Almonds and walnuts provide heart-healthy fats and magnesium, but limit portions to avoid overloading the stomach.
Healing your gut starts in your kitchen. With these power-packed foods—rooted in science and nurtured through nature—you can nourish your body, reduce inflammation, and promote deep healing. At Claudia’s Concept, food isn’t just fuel. It’s your strongest medicine.

Natural Remedies and Healing Supplements to Combat H. Pylori Effectively
When it comes to nourishing your digestive system and supporting your body through an H. pylori infection, your kitchen and supplement cabinet can be as valuable as your prescription. I’ve seen remarkable results at Claudia’s Concept by integrating nature’s pharmacy with clinically-proven therapies. Let’s dive into healing the gut from the inside out—with targeted natural remedies that work in synergy with medication to speed up recovery and reduce discomfort.
Green Tea: Sip Your Way to a Stronger Gut
One of the most subtle yet powerful allies in managing H. pylori is green tea. Rich in catechins, particularly epigallocatechin gallate (EGCG), green tea exhibits significant antibacterial activity against H. pylori. A study published in the journal Diagnostics (2020) illustrated that subjects who regularly drank green tea had reduced H. pylori colonization and lower inflammation markers in the gastric mucosa.
Enjoying two to three cups of high-quality organic green tea daily can tilt the balance in your favor—not just by directly inhibiting bacterial growth but also by calming the digestive tract.
Honey: Natural Antimicrobial Power
Nature’s sweet remedy, raw unprocessed honey—especially manuka honey—has demonstrated antimicrobial action against H. pylori. A comparative microbiology study from Archives of Medical Research (2006) found that honey inhibits the growth of various H. pylori strains in vitro.
At Claudia’s Concept, I often recommend incorporating one teaspoon of manuka honey on an empty stomach in the morning. This simple addition can soothe the stomach lining and serve as a daily dose of antibacterial support.
Garlic: Nature’s Broad-Spectrum Antibiotic
Garlic’s sulfur-containing compounds—like allicin—make it another weapon against H. pylori. Not only does garlic inhibit bacterial proliferation, but it also modulates immune responses. A randomized clinical trial published in the journal Phytomedicine (2014) showed that patients who consumed garlic extract twice daily for three weeks had significantly decreased bacterial load compared to the placebo group.
Finely minced raw garlic, consumed with meals or in a small yogurt-based dip, brings both antimicrobial and gut-immune fortifying effects.
Zinc and Vitamin C: Repair and Protect the Gut Lining
- pylori doesn’t only colonize the stomach—it damages the integrity of the gut lining. That’s where zinc and vitamin C step in. Zinc is essential for mucosal repair and immune modulation, while vitamin C helps reduce oxidative stress caused by infection.
A clinical trial in the World Journal of Gastroenterology (2013) found that supplementing vitamin C alongside standard triple therapy increased eradication success by more than 10%. Meanwhile, deficiencies in zinc are commonly associated with prolonged gut inflammation.
- Zinc dosage: 30–45 mg elemental zinc per day
- Vitamin C dosage: 500–1000 mg per day, taken with meals
These two antioxidants accelerate stomach lining repair—ensuring that once the bacteria are cleared, your gut has the tools to rebuild resilience swiftly.
Enhancing Therapy: Natural Remedies Plus Medication = Results
Here’s the truth—natural remedies shine brightest when they complement medical treatment. H. pylori eradication often requires antibiotics. By adding gut-healing foods and supplements, you create a holistic strategy that tackles both the infection and the collateral damage it causes.
I work closely with medical professionals to ensure that everything recommended through Claudia’s Concept aligns with prescribed therapies. For clients undergoing drug treatment, integrating gentle yet potent natural remedies reduces side effects, supports compliance, and shortens recovery time.
Ever tried combining green tea with probiotics or pairing garlic with a zinc-rich meal? If you haven’t, now’s the perfect time to practice nourishing your gut with precision. Think about which remedies resonate with your lifestyle and take that first step toward strengthening your gut health.
What Not to Eat: Foods to Avoid with an H. Pylori Infection
Healing your gut from H. pylori isn’t just about what you’re adding to your plate—it’s also about what needs to go. At Claudia’s Concept, we know certain foods actively irritate the stomach lining, slow your recovery, or even interfere with medications used in the treatment. That’s why identifying and eliminating these trigger foods is just as powerful as embracing healing ones.
Stomach Lining Offenders: What You Should Avoid
When H. pylori infects the stomach, it causes inflammation of the mucosal lining. Ingredients that further irritate or inflame this lining can intensify symptoms and extend the recovery phase. Here’s what you’ll want to cut out or dramatically reduce:
- Spicy and acidic foods: These cause direct irritation to the stomach wall. Chili peppers, hot sauces, vinegar-based dressings, citrus fruits, and raw tomatoes are common culprits. Capsaicin—the compound responsible for chili’s heat—provokes acid production, disrupting the healing process.
- Fried and fatty foods: High-fat meals—especially those rich in unhealthy oils or deep-fried—delay gastric emptying. This keeps your stomach acidic for longer, exacerbating existing inflammation. Studies show saturated fats can increase gastric mucosal permeability, making it easier for H. pylori to cause damage.
- Caffeinated beverages: Coffee, black tea, and energy drinks stimulate gastric acid secretion. Even decaffeinated varieties can irritate sensitive digestive systems due to other natural compounds. Avoid these especially during acute flare-ups.
- Alcohol: Ethanol, found in all alcoholic beverages, directly damages epithelial cells in your stomach. It also interferes with antibiotics commonly prescribed to combat H. pylori. The combination can reduce drug efficacy and prolong infection duration.
- Processed and convenience foods: These often contain trans fats, excessive sodium, sugar, and preservatives—all of which contribute to systemic inflammation. Sodium nitrate, used to preserve meats like bacon and sausages, has shown potential to aggravate gastric lesions in animal studies.
- Carbonated drinks: Soda and fizzy beverages increase bloating and stomach pressure. The carbon dioxide gas they release causes distension, which can worsen the discomfort already caused by H. pylori-induced gastritis.
Pay Attention to Personal Triggers
While the foods mentioned above are commonly problematic, your body might have its own sensitivities. Some people find dairy irritating, while others may respond badly to onions or garlic. Keeping a detailed food and symptom journal for at least two weeks can shed light on hidden culprits. Track what you eat, when you eat it, and any symptoms that develop. Then identify patterns—Claudia’s Concept uses this data-driven approach for every client struggling with chronic gastric issues.
Working through these eliminations with intention and accuracy supports faster healing and minimizes discomfort. The fewer irritants your stomach has to combat, the better your chances of keeping both symptoms and bacteria under control.
Hydration and Gut Health: How Fluids Can Fuel Your Recovery from H. Pylori
Hydration isn’t just about quenching your thirst—it’s deeply connected to how your body digests, heals, and flushes out toxins, especially when you’re dealing with an H. pylori infection. A well-hydrated gut supports smoother digestion, maintains the integrity of the stomach lining, and optimises the body’s natural detoxification processes. At Claudia’s Concept, I work with clients to ensure that we don’t just focus on food, but also on how fluid intake supports gut health on a cellular level.
Why Proper Hydration Matters During H. Pylori Treatment
When H. pylori takes hold in the stomach lining, it often disrupts the acid balance, leading to symptoms like bloating, nausea, and indigestion. Water helps regulate gastric acidity and keeps mucosal tissues hydrated, which reduces irritation. In fact, studies published in The American Journal of Physiology show that dehydration can reduce mucosal blood flow and impair gut barrier function, making it harder for your stomach to heal.
Moreover, during antibiotic treatment for H. pylori, hydration becomes even more crucial because your kidneys and liver need adequate water to process and eliminate byproducts of both the bacteria and medications. Sufficient water intake supports healthy peristalsis, promotes nutrient absorption, and prevents constipation—issues that often arise when your digestive tract is inflamed.
Best Sources of Hydration for a Healing Gut
- Filtered Water: Aim for about 2.5 to 3 litres throughout the day, depending on your body weight and activity level. Sipping water gradually—especially between meals—helps keep digestion efficient without diluting stomach acid.
- Herbal Teas: Chamomile and licorice root teas are two of my favourite recommendations at Claudia’s Concept. Chamomile soothes inflammation and supports better sleep, while licorice root contains glycyrrhizin, which has been shown in Phytotherapy Research Journal to inhibit H. pylori growth.
- Coconut Water: In moderation, it provides natural electrolytes like potassium and magnesium. It also offers light hydration without artificial additives—ideal after a workout or a long day in the sun.
Fluids to Avoid When Managing H. Pylori
- Sugary Drinks: Soft drinks, fruit punches, and flavoured iced teas flood your system with refined sugars, which can promote inflammation and worsen gastric symptoms. A 2019 study in Gut Microbes linked high-sugar diets with lower microbial diversity and weaker gut immunity.
- Carbonated Sodas: Carbonation increases bloating and pressure in the stomach, which can intensify discomfort in those with gastritis or ulcers. Plus, many sodas contain phosphoric acid and caffeine, which are harsh on an already compromised stomach lining.
Take a moment to reflect: are you drinking enough water daily to support your gut’s recovery? Investing in proper hydration is one of the simplest but most powerful steps you can take. It’s a pillar in our gut-healing protocols at Claudia’s Concept, and it always delivers results.
Long-Term Habits to Prevent Recurrence of H. Pylori
When it comes to staying free from H. pylori after treatment, the journey doesn’t just end with antibiotics or a temporary diet shift. Long-lasting gut health requires consistency, attention to detail, and conscious daily choices that support a balanced digestive environment. The lifestyle and food habits you maintain post-treatment will decide whether this bacterium makes a comeback or stays gone for good.
How Smart Dietary Habits Keep H. Pylori at Bay
Let’s talk about stomach acid. H. pylori thrives in a weakened, unbalanced gastric environment. While many assume that lowering acid is helpful, in reality, low stomach acid can create optimal conditions for H. pylori to recolonize. That’s why one of the nutritional pillars at Claudia’s Concept is targeting optimal acid balance through foods that enhance digestive function without causing irritation.
Fermented vegetables like kimchi and sauerkraut, for example, contain lactic acid bacteria that naturally help regulate the stomach’s ecosystem. Research published in Frontiers in Microbiology has shown that strains like Lactobacillus plantarum can inhibit H. pylori adhesion and promote gastric healing.
Incorporating prebiotic fibers found in onions, asparagus, and garlic supports the production of short-chain fatty acids, which reduce inflammation and improve mucosal barrier function — directly limiting the chance of reinfection.
Key Behavioral Habits That Strengthen Stomach Integrity
- Eat Slowly and Chew Each Bite Thoroughly – Digestion begins in the mouth. By chewing properly, you trigger salivary enzymes that start breaking down food, reducing stress on your stomach and increasing acid production efficiency. This simple practice improves nutrient absorption and protects against bacterial overgrowth.
- Avoid Late-Night Eating – Eating late disrupts your digestive rhythm and suppresses gastric acid secretion during its natural cycle. A study in the American Journal of Gastroenterology found that late-night meals may prolong gastric emptying and heighten the risk of acid reflux, both of which irritate the stomach lining.
- Maintain a Healthy Body Weight – Excess body fat increases abdominal pressure and alters the bacterial balance of the gut. According to a 2021 review in Gut Microbes, visceral fat contributes to chronic low-grade inflammation — a key enabler of H. pylori persistence. Sustainable weight management eliminates one of the major risk factors for recurrence.
Post-Treatment: What to Reintroduce, What to Rethink
After completing treatment and beginning to feel better, there’s often a temptation to return to “normal eating.” But let’s redefine what “normal” should mean for your gut. At Claudia’s Concept, we focus on not just eliminating disease, but building long-term habits that embody health. This means being intentional about the foods you invite back into your daily meals.
- Gradually Reintroduce: Raw vegetables, whole grains, and mild spices — start slow and observe your body’s feedback. Cooked vegetables should remain the core in the beginning because they’re easier to digest.
- Limit or Remove Long-Term: Processed meats, sugary desserts, ultra-refined carbs, and heavily caffeinated drinks. These not only irritate the stomach lining but also disrupt gut flora, giving H. pylori a chance to come back.
Every decision made at the table either nurtures balance or fuels imbalance. Your gut doesn’t work in isolation; it’s a responsive system built on the consistency of your choices. The right routine — supported by whole foods, mindful eating, and inflammation-reducing behaviors — creates an environment that leaves no room for H. pylori to return.
H. pylori is a spiral-shaped bacterium that lives in the stomach lining. It weakens the protective mucous layer, increases inflammation, and can lead to symptoms like bloating, pain, nausea, indigestion, and in severe cases, ulcers.
Yes. While medication is usually required to eradicate the bacteria, diet plays a major role in healing the stomach lining, reducing inflammation, and restoring healthy gut flora. Specific foods can soothe the digestive tract and help limit bacterial growth.
Foods rich in antioxidants, probiotics, omega-3 fats, and soothing nutrients — such as berries, leafy greens, broccoli sprouts, yogurt, kefir, ginger, turmeric, bone broth, and manuka honey — support healing and gut repair.
Avoid spicy foods, acidic foods, fried and fatty foods, caffeine, alcohol, carbonated drinks, and processed meats. These irritate the stomach lining and can worsen symptoms or slow recovery.
Yes. Green tea catechins, raw garlic, manuka honey, zinc, and vitamin C can support immune strength, reduce inflammation, and help the gut heal when used alongside medical treatment. They should complement — not replace — prescribed antibiotics.